
Do you wake up with a sore jaw or notice your teeth feeling worn down? You might be experiencing bruxism, a condition where you grind or clench your teeth, especially during sleep.
This article explores the symptoms and causes of teeth grinding at night, shedding light on how stress and anxiety can contribute. Understanding bruxism can help you manage and prevent further damage to your teeth and jaw, improving your dental health.
Bruxism is the involuntary clenching or grinding of the upper and lower teeth, occurring without food in the mouth. It represents a harmful non-physiological movement of the stomatognathic system, characterized by the clenching or grinding of teeth resulting from the contraction of various jaw muscles, including the masseter and temporal muscles.
Sleep-related bruxism affects 15-40% of children and 8-10% of adults, as indicated by cross-sectional survey studies and self-reports. In children, bruxism typically emerges after the eruption of front teeth. Awake bruxism is more common in females than males, but sleep bruxism does not show a gender preference. As individuals age, the prevalence of bruxism tends to decrease. For adults over 65, some studies suggest an incidence of about 3%.
Related content:
What It Means When Toddlers Grind Their Teeth
Bruxism is classified into two categories based on age: children and adults. It is also categorized by the time of occurrence, distinguishing between awake bruxism and sleep bruxism.
Furthermore, bruxism exhibits distinct characteristics, including clenching, grinding, and a mixed mode involving both clenching and grinding.

The causes of bruxism include stress, anxiety, lifestyle factors, medical conditions, and psychological factors. Teeth grinding, especially at night, can be triggered by stress and anxiety during the day. Lifestyle choices like high caffeine intake, alcohol use, and smoking can also contribute to bruxism.
The causes of bruxism are complex, involving various factors:
If you experience teeth grinding at night, psychological factors can play a significant role in exacerbating this condition. Here are some key points to consider regarding the relationship between sleep bruxism and psychological factors:
Consider how medical factors can influence bruxism, affecting your dental health and overall well-being. Medical conditions like GERD, epilepsy, and sleep-related disorders can contribute to teeth grinding during sleep.
Symptoms such as flattened, chipped, or loose teeth, worn enamel, and jaw pain may indicate bruxism related to these medical factors. Diagnosis involves dental exams and symptom inquiries, leading to treatments like stress management, dental splints, and behavioral therapies.
In severe cases, a multidisciplinary approach may be necessary for effective treatment. Regular dental care is crucial in monitoring and managing bruxism stemming from medical factors.
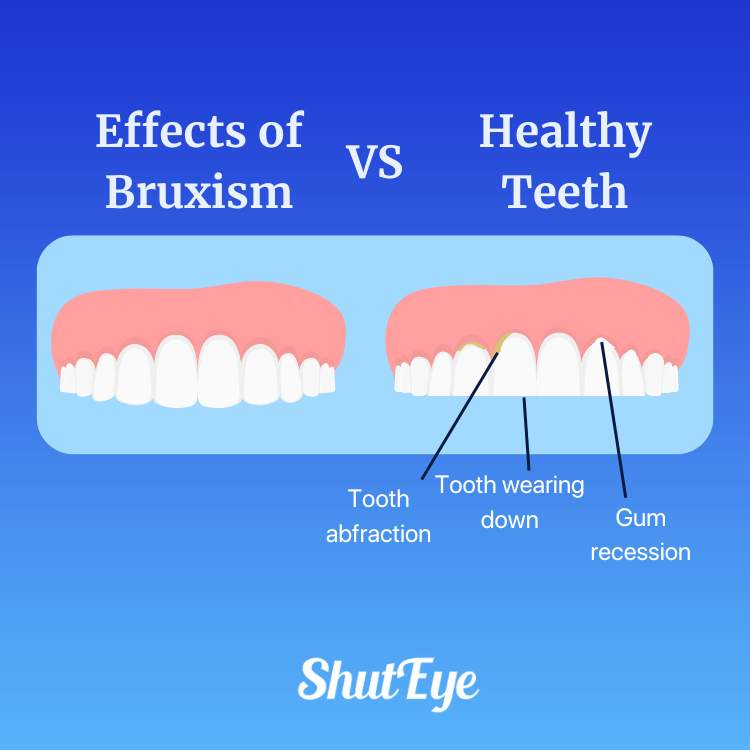
When experiencing bruxism, you may notice symptoms such as flattened, chipped, or loose teeth. These signs and symptoms can indicate that you’re grinding or clenching your teeth, especially at night.
Here are three common indicators of bruxism:
When teeth grinding occurs, it can lead to various adverse effects on your oral health and overall well-being. Grinding your teeth during sleep can result in fracturing, loosening, or loss of teeth, wearing teeth down to stumps, and the need for bridges, crowns, root canals, implants, or dentures. Additionally, the impact on the jaws and temporomandibular joint (TMD/TMJ) can cause changes in facial appearance. To address these issues, identifying the cause of teeth grinding and seeking treatments such as mouth guards, dental corrections, stress reduction techniques, and proper sleep hygiene practices are crucial. Regular monitoring by a dentist is essential for managing the effects of teeth grinding effectively.
The most reliable diagnostic evidence for sleep-related bruxism comes from a history of teeth grinding during sleep, corroborated by parents, caregivers, or bed partners. In cases of uncertain diagnosis, bruxers’ reports, clinical interviews, clinical examination, intraoral appliances, or recording of muscle activity can aid in diagnosing sleep bruxism.
Physicians should ask bruxers about risk and exacerbating factors, including signs of poor sleep quality, symptoms of obstructive sleep apnea (e.g., loud snoring, witnessed pauses in breathing), and excessive caffeine or alcohol intake. Evaluating the medication list for potential contributors, including antipsychotic and serotonergic drugs, is also essential.
During regular dental exams, dentists may check for signs of bruxism, including tenderness in jaw muscles and dental abnormalities like broken or missing teeth.
Understanding these diagnostic methods is crucial for comprehensive assessment and effective management of sleep-related bruxism.
Many individuals with sleep-related bruxism may not require specific treatment, as occasional bruxism is common, especially during childhood, and often asymptomatic. However, for those with frequent or symptomatic bruxism, various therapies are available. To address bruxism effectively, consider utilizing mouth guards, dental corrections, stress reduction techniques, and proper sleep hygiene practices as part of the treatment options. Here are some strategies to help reduce bruxism:
The primary goal of treatment is to eliminate bruxism symptoms, reduce muscle tension, and safeguard the function of the stomatognathic system. Tailoring the approach to each individual’s needs and considering various therapeutic options can lead to effective management of sleep-related bruxism.
Utilize preventive measures to manage bruxism by incorporating stress reduction techniques and maintaining proper sleep hygiene practices.
Recognize symptoms like flattened or chipped teeth, worn enamel, and jaw tightness as indicators of teeth grinding. Address causes such as stress, anxiety, and lifestyle factors by practicing stress management techniques like deep breathing or listening to ShutEye® App.
Implement prevention techniques such as using a custom mouthguard at night to protect teeth from grinding during sleep. Prioritize relaxation methods before bedtime to reduce nighttime grinding, including warm cloth application to relax jaw muscles.
Ensure children practice good dental habits and stress-relief activities to prevent teeth grinding. Regular dental check-ups and consultations can aid in monitoring and managing bruxism effectively.

Regularly, you may experience teeth grinding at night due to various risk factors associated with bruxism. These risk factors include:
Understanding these risk factors can help in identifying potential causes of teeth grinding and may guide you toward seeking appropriate interventions to manage bruxism effectively.
Complications of bruxism can include severe tooth, jaw, or restoration damage. When left untreated, the symptoms of teeth grinding, such as flattened or chipped teeth, worn enamel, and jaw pain, can worsen, leading to long-term issues.
Constant grinding can cause tension-type headaches, facial pain, and even temporomandibular joint disorders, characterized by clicking sounds in the jaw. Over time, the continuous pressure on teeth and jaw muscles from bruxism can result in fractures, loose teeth, or the need for extensive dental work like bridges, crowns, or implants.
Monitoring and addressing teeth grinding promptly can help prevent these complications and preserve your dental health and overall well-being.

In conclusion, understanding the causes and symptoms of bruxism is crucial in managing this common dental issue.
By addressing psychological and medical factors, seeking appropriate treatment, and implementing preventive measures, you can protect your teeth and jaw from the damaging effects of teeth grinding at night.
Taking steps to reduce stress, anxiety, and other risk factors can help you improve your overall dental health and prevent complications associated with bruxism.
Sleep, (2016), Sleep Bruxism-Tooth Grinding Prevalence, Characteristics and Familial Aggregation: A Large Cross-Sectional Survey and Polysomnographic Validation https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5070759/
J Indian Prosthodont Soc. (2010) Bruxism: A Literature Review https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3081266/
Shetty S, Pitti V, Satish Babu CL, Surendra Kumar GP, Deepthi BC. Bruxism: a literature review. J Indian Prosthodont Soc. 2010 Sep;10(3):141-8. doi: 10.1007/s13191-011-0041-5. Epub 2011 Jan 22. PMID: 21886404; PMCID: PMC3081266.
Khoury S, Carra MC, Huynh N, Montplaisir J, Lavigne GJ. Sleep Bruxism-Tooth Grinding Prevalence, Characteristics and Familial Aggregation: A Large Cross-Sectional Survey and Polysomnographic Validation. Sleep. 2016 Nov 1;39(11):2049-2056. doi: 10.5665/sleep.6242. PMID: 27568807; PMCID: PMC5070759.
National Sleep Foundation (U.S.). The Link Between Sleep Apnea and Teeth Grinding. https://www.sleepfoundation.org/sleep-apnea/link-between-sleep-apnea-and-teeth-grinding Updates 10/20/2023. Accessed 12/18/2023.
NHS (U.K.). Teeth Grinding (Bruxism) https://www.nhs.uk/conditions/teeth-grinding/ Last reviewed 6/27/2022. Accessed 12/18/2023.