

Curious about how genetics impact narcolepsy?
Today, we will explore how genes play a role in this sleep disorder and what it means for those affected.
Gain valuable insights into diagnosis, treatment, and future advancements in managing narcolepsy.
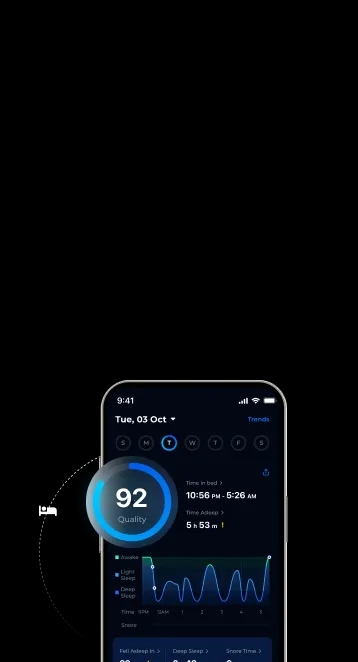
Narcolepsy is a neurological disorder characterized by uncontrollable and excessive daytime sleepiness, often accompanied by sudden and temporary loss of muscle tone (cataplexy), vivid hallucinations, and brief episodes of paralysis when falling asleep or upon waking (sleep paralysis). It is a chronic condition that affects the brain’s ability to regulate sleep-wake cycles, leading to disrupted sleep patterns and frequent transitions between wakefulness and various stages of sleep.
While the exact cause of narcolepsy is not fully understood, it is believed to involve a combination of genetic predisposition and environmental factors that affect the brain’s production of orexin, a neurotransmitter responsible for promoting wakefulness. Narcolepsy can significantly impact daily functioning and quality of life, but management strategies, including medications and lifestyle adjustments, can help individuals effectively manage their symptoms.
When exploring the genetic basis of narcolepsy, you may find that certain individuals are more susceptible due to a genetic component.
Narcolepsy, especially type 1, is strongly linked to genetics, often involving the HLA-DQB1*06:02 gene variant. This specific gene variant is prevalent in most type 1 narcolepsy cases and is present in around 20% of individuals without narcolepsy.
Moreover, certain rare types of narcolepsy can be autosomal dominant, passing from parent to child. Understanding these genetic factors is crucial in diagnosing and treating narcolepsy effectively.
Explore the significant role of HLA in narcolepsy to understand its genetic connection better. The HLA-DQB1*06:02 gene variant plays a crucial role in narcolepsy, impacting susceptibility and development.
To grasp the emotional impact of this genetic link, consider the following:
Understanding the autoimmune factors in narcolepsy’s development is key to unraveling its complexities.
In narcolepsy type 1 (NT1), an autoimmune process targets and damages neurons containing hypocretin, a crucial neurotransmitter involved in regulating wakefulness and sleep.
This autoimmune reaction is often triggered by a combination of genetic predisposition, environmental factors, and potential immune system dysregulation.
The presence of the HLA-DQB1*06:02 gene variant is strongly associated with NT1, indicating a genetic susceptibility to this autoimmune response.
Research suggests that specific influenza strains and other environmental triggers may contribute to the development of narcolepsy by initiating or exacerbating the autoimmune process.
Inheriting narcolepsy involves genetic factors interacting with environmental triggers, impacting the development and manifestation of the disorder. Understanding how narcolepsy can be passed down can provide insights into its management and potential risk factors. Here are some points to consider:
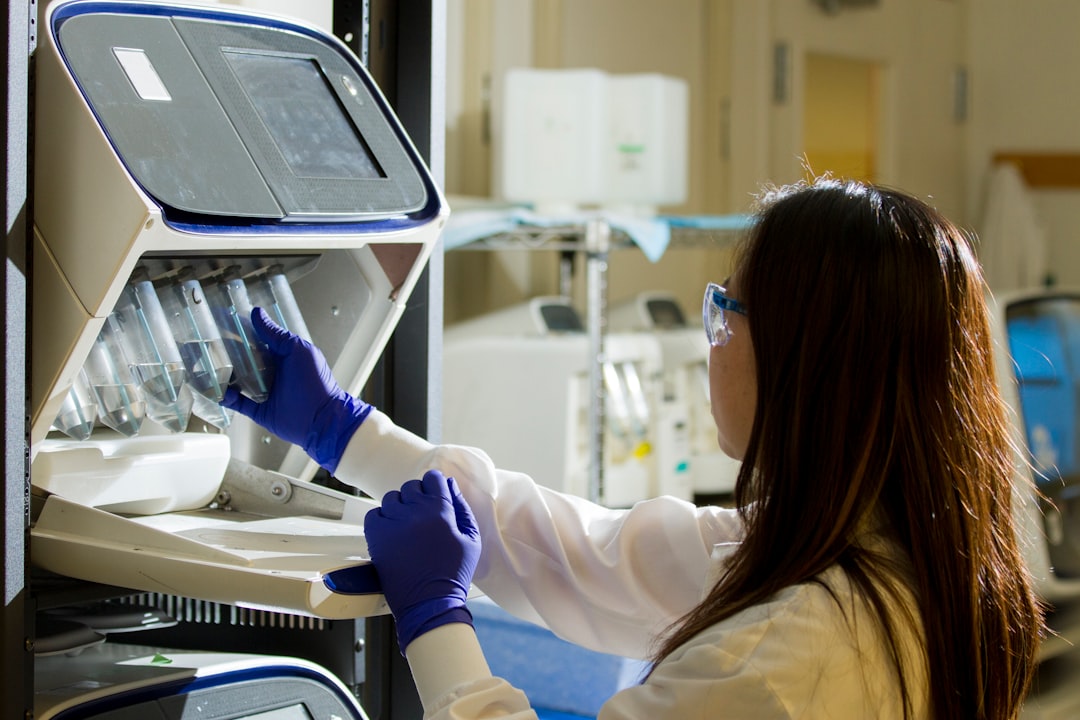
If you suspect narcolepsy runs in your family, genetic testing can provide valuable insights into your risk factors. By understanding the genetic components of narcolepsy, you can better comprehend your predisposition to this condition. Genetic testing can identify specific gene variants associated with narcolepsy, aiding in early detection and personalized treatment plans. Below is a table summarizing key genes involved in narcolepsy:
| Gene | Association | Prevalence in Narcolepsy |
|---|---|---|
| HLA-DQB1*06:02 | Strongly linked to narcolepsy type 1 | Present in most NT1 cases and 20% without narcolepsy |
| Hypocretin Neurons | Damage can lead to narcolepsy | Associated with NT1 and cataplexy |
| Autosomal Dominant Genes | Rare types can be inherited | Pass from parent to child |
Genetic testing can offer valuable information for individuals with a family history of narcolepsy, aiding in proactive management strategies.
Explore the environmental triggers that can influence narcolepsy development. Environmental factors can significantly impact the onset and progression of narcolepsy. Consider the following emotional triggers:
Understanding these environmental triggers is crucial in managing narcolepsy effectively and improving quality of life. By being mindful of these factors, you can better navigate the challenges associated with narcolepsy.
You may also like:
The Link Between Narcolepsy and ADHD
Understanding the genetic variations in narcolepsy subtypes can provide valuable insights into the condition’s underlying mechanisms and potential treatment approaches. Narcolepsy is categorized into two main subtypes: type 1 (NT1) and type 2 (NT2). Here’s a simplified breakdown of the genetic aspects associated with each subtype:
| Narcolepsy Subtype | Genetic Characteristics | Associated Features |
|---|---|---|
| Type 1 (NT1) | Strong link to HLA-DQB1*06:02 gene variant | Orexin deficiency, autoimmune reaction involvement |
| Type 2 (NT2) | Genetic factors less understood | Less commonly associated with orexin deficiency |
Future genetic research in narcolepsy aims to uncover novel genetic markers associated with specific subtypes to enhance personalized treatment strategies. As this research progresses, here are some emotional responses you might experience:
As you reflect on the genetic link in narcolepsy, you realize the intricate role genes play in predisposing individuals to this complex sleep disorder.
Understanding the genetic basis of narcolepsy sheds light on its diagnosis, treatment, and potential advancements in managing symptoms.
By unraveling the mysteries behind narcolepsy subtypes and their genetic underpinnings, you gain valuable insights that could lead to improved care for those affected by this neurological condition.
Keep exploring the genetic landscape of narcolepsy for further discoveries and advancements.
A.D.A.M. Medical Encyclopedia. (2021, July 26). Narcolepsy. MedlinePlus., Retrieved September 29, 2023, from https://medlineplus.gov/ency/article/000802.htm
Genes and Disease. Narcolepsy. [Internet]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK22236/. Accessed [Fri 4 Apr 2024].
Ollila H. M. (2020). Narcolepsy type 1: what have we learned from genetics?. Sleep, 43(11). https://pubmed.ncbi.nlm.nih.gov/32442260/
Shimada, M., Miyagawa, T., Toyoda, H., Tokunaga, K. & Honda, M. Epigenome-wide association study of DNA methylation in narcolepsy: an integrated genetic and epigenetic approach. Sleep 41, (2018).