
Do you struggle with the constant urge to move your legs, especially at night? Restless Leg Syndrome (RLS) might be the cause of those uncomfortable sensations. This article delves into the symptoms, causes, and treatment options for RLS.
From aching legs to disruptions in daily life, managing RLS can be tough. Learn how genetics, iron deficiency, and medications play a role in RLS, and discover coping strategies to help relieve your symptoms, improve your quality of life, and sleep better.
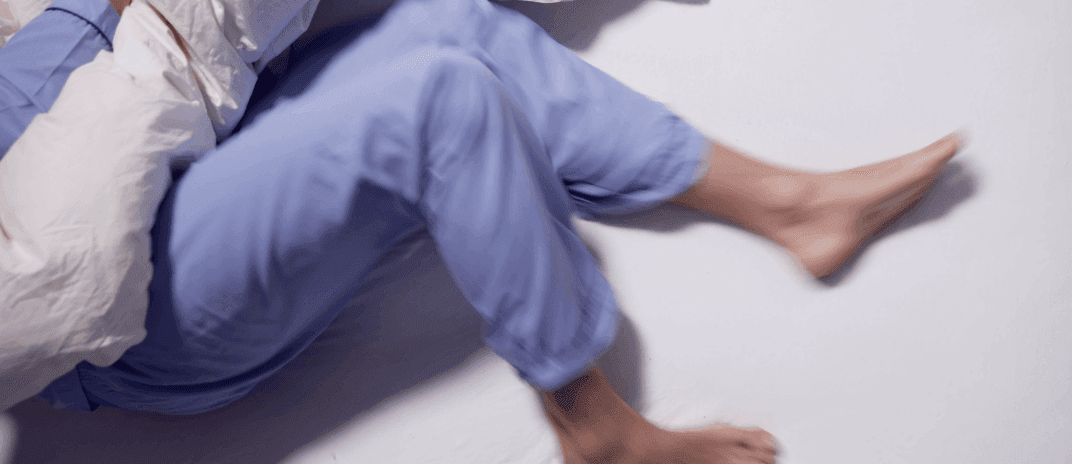
Restless Legs Syndrome (RLS), also known as Willis-Ekbom Disease (WED), is a condition where the legs feel highly uncomfortable while sitting or lying down. Individuals with RLS experience an irrepressible urge to move their legs, often accompanied by abnormal sensations like burning, tingling, aching, or the feeling of “insects crawling under the skin.” These sensations are transiently relieved by any small movement, and RLS exhibits a strong circadian influence, with symptoms worse in the evening.
RLS is categorized into two main types: Primary and Secondary RLS. Primary RLS, also termed idiopathic, occurs without any underlying medical issues. On the other hand, secondary RLS is triggered by medical problems such as pregnancy, alcohol addiction, iron deficiency, among others.
The prevalence rate of Restless Legs Syndrome (RLS) ranges from 5% to 15% in the general population. Approximately 2.5% of adults with RLS experience severe symptoms requiring medical intervention. Several risk factors associated with RLS include being female, pregnancy, low iron levels, lower socioeconomic status, poor health, and older age. Additionally, common comorbidities include Parkinson’s disease, a positive family history of RLS, and psychiatric disorders. It’s worth noting that RLS can pose challenges, making both sleeping and traveling difficult and uncomfortable.
If you experience an urge to move your legs, especially at night, you might be exhibiting symptoms of Restless Leg Syndrome (RLS). These cases of restless legs syndrome often manifest as uncomfortable sensations in your legs, such as itching, pulling, or aching, creating an overpowering need to shift or move your legs.
The sensations can vary in intensity, typically worsening in the evening and improving in the early morning. It’s essential to note that these symptoms are neurological in nature and can impact your daily life, especially disrupting your sleep.
If you find yourself dealing with these uncomfortable sensations and urges, seeking evaluation and guidance from a healthcare professional can help in managing and addressing the symptoms of restless legs syndrome effectively.
The causes of restless legs syndrome can be attributed to various factors, including an imbalance in brain chemical dopamine and identified genetic sites associated with RLS.
Understanding these causes can shed light on why individuals experience the urge to move their legs and the uncomfortable sensations associated with restless leg syndrome.
While not usually connected to serious medical conditions, factors like dopamine levels and genetic influences play a significant role in the development of RLS. Seeking medical guidance and exploring management options can help alleviate the symptoms and improve the quality of life.

Exploring potential risk factors for developing restless legs syndrome involves considering family history, low iron levels, and related conditions like neuropathy and renal disease. Individuals with a family history of restless leg syndrome are at a higher risk of developing the condition. Low iron levels in the brain can also contribute to the onset of RLS symptoms. Additionally, medical conditions such as neuropathy and renal disease are associated with an increased likelihood of experiencing restless legs syndrome.
To diagnose restless legs syndrome, consider family history, iron levels, and related conditions. When evaluating for RLS, healthcare providers may:
Seeking a healthcare professional’s guidance is essential for an accurate diagnosis and appropriate treatment plan. By addressing these key factors, you can work towards managing the urge to move your legs, improving your quality of life, and finding relief from the discomfort associated with restless leg syndrome.
Consider involving your healthcare provider to explore effective treatment options for managing restless legs syndrome. Treatment for RLS aims to alleviate symptoms and improve quality of life. Medications like dopaminergic agents can help regulate dopamine levels in the brain, reducing leg discomfort.
Iron supplements may be prescribed if low iron levels are detected, as this imbalance can trigger RLS symptoms. Lifestyle adjustments such as avoiding stimulants like caffeine and alcohol, maintaining a regular sleep schedule, and engaging in moderate exercise can also aid in symptom management.
Additionally, addressing any underlying medical conditions that may worsen RLS, like peripheral neuropathy or kidney failure, is essential for comprehensive treatment. Collaborate with your healthcare provider to create a personalized treatment plan tailored to your specific needs
Discuss with your healthcare provider potential medications for managing restless legs syndrome, focusing on alleviating symptoms and enhancing your quality of life.
These medications aim to target the underlying causes of restless legs syndrome, such as dopamine imbalance and nervous system dysfunction, to alleviate the sensations and urge to move your legs, ultimately improving your daily life and sleep quality. Be sure to follow your healthcare provider’s recommendations for the most effective treatment plan.

Implementing a balanced exercise routine can significantly aid in managing restless legs syndrome, contributing to symptom alleviation and enhancing overall well-being. Lifestyle changes play a crucial role in the management and prevention of RLS symptoms. Making simple adjustments can have a positive impact on your condition. Here are some effective lifestyle changes for RLS:
| Lifestyle Changes | Description |
|---|---|
| Regular Exercise | Symptoms usually disappear after moderate physical activity. |
| Healthy Sleep Habits | Maintain a consistent sleep schedule to improve rest and minimize RLS triggers. |
| Balanced Diet | Consume iron-rich foods and avoid excessive caffeine and alcohol intake. |
Utilize lifestyle adjustments and coping techniques to effectively manage the symptoms of Restless Legs Syndrome (RLS). Here are some strategies to help you cope with the sensations and challenges that RLS presents:
To understand the impact of Restless Legs Syndrome on your quality of life, consider the disruptive nature of the condition’s symptoms. Moderate to severe RLS can lead to uncomfortable sensations in your legs, affecting your ability to rest and causing nighttime leg twitching that disrupts your sleep.
This disturbance in your sleep pattern can result in decreased quality of life, potentially leading to daytime fatigue, irritability, and difficulty concentrating on tasks. Seeking proper treatment for RLS and effectively managing the condition is crucial in minimizing its impact on your daily life.
Restless Legs Syndrome (RLS) is associated with several complications, including:
Understanding the relationship between Restless Leg Syndrome and Periodic Limb Movement of Sleep is essential for effectively managing these conditions. Here are key points to consider:
Exploring the latest research findings and advancements in treating Restless Leg Syndrome can provide valuable insights into managing this neurological disorder effectively. Recent studies have focused on understanding the connection between restless legs syndrome (RLS) and other neurological disorders like stroke, investigating how leg movements and sensations in the legs are linked to RLS symptoms.
Advances in diagnosis and treatment have led to improved methods for accurately identifying RLS, such as utilizing advanced imaging techniques to study brain signaling pathways and genetic influences. Researchers are also exploring new treatment options, including innovative medications and therapies, to enhance symptom management and overall quality of life for individuals living with RLS.
Stay informed about these developments to better navigate the complexities of RLS management.
Behavior Management:
Interventions involving behavioral changes include:
Monitoring Diary:
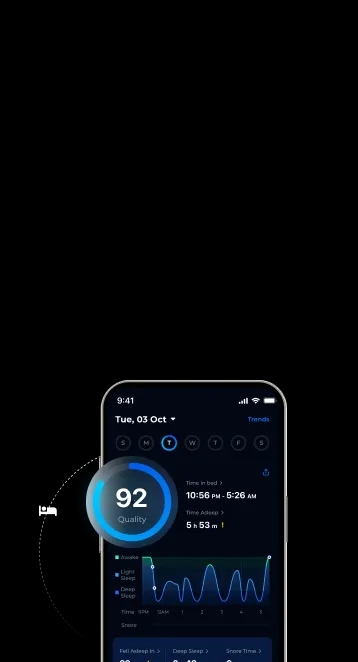
During RLS treatment, a monthly efficacy assessment is conducted to determine whether symptoms have improved or disappeared and whether daily life has returned to normal.
Experts recommend the following tasks to prevent RLS:
Continue your journey in managing Restless Legs Syndrome by exploring the support resources available to help you cope with this neurological disorder.
Here are some valuable support resources for RLS:
In conclusion, if you find yourself struggling with the urge to constantly move your legs, especially at night, it may be due to Restless Legs Syndrome (RLS). By recognizing the symptoms, causes, and treatment options for RLS, you can take proactive steps towards managing this challenging condition.
With the right support and care, you can improve your quality of life and get a good night’s rest. Don’t hesitate to seek help and explore coping strategies to alleviate your symptoms.
Ther Clin Risk Manag. (2006), Restless leg syndrome: is it a real problem? https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1936366/
Ann Thorac Med. (2015), Prevalence of restless legs syndrome and associated risk factors among middle-aged Saudi population, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4518350/
Iran J Neurol. (2016), Treatment of restless legs syndrome/Willis-Ekbom disease with selenium, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5392199/
Cotter PE, O'Keeffe ST. Restless leg syndrome: is it a real problem? Ther Clin Risk Manag. 2006 Dec;2(4):465-75. doi: 10.2147/tcrm.2006.2.4.465. PMID: 18360657; PMCID: PMC1936366.
Ulfberg J, Stehlik R, Mitchell U. Treatment of restless legs syndrome/Willis-Ekbom disease with selenium. Iran J Neurol. 2016 Oct 7;15(4):235-236. PMID: 28435634; PMCID: PMC5392199.
Ekbom K, Ulfberg J. Restless legs syndrome. J Intern Med. 2009;266(5):419–31. [Google Scholar]