
Insomnia, also known as sleeplessness, stands out as one of the most prevalent sleep disorders among adults. It often leads to disruptive sleep patterns that impact daily life. Various factors, including stress, medications, and an individual’s sleep habits and environment, can contribute to the development of insomnia.
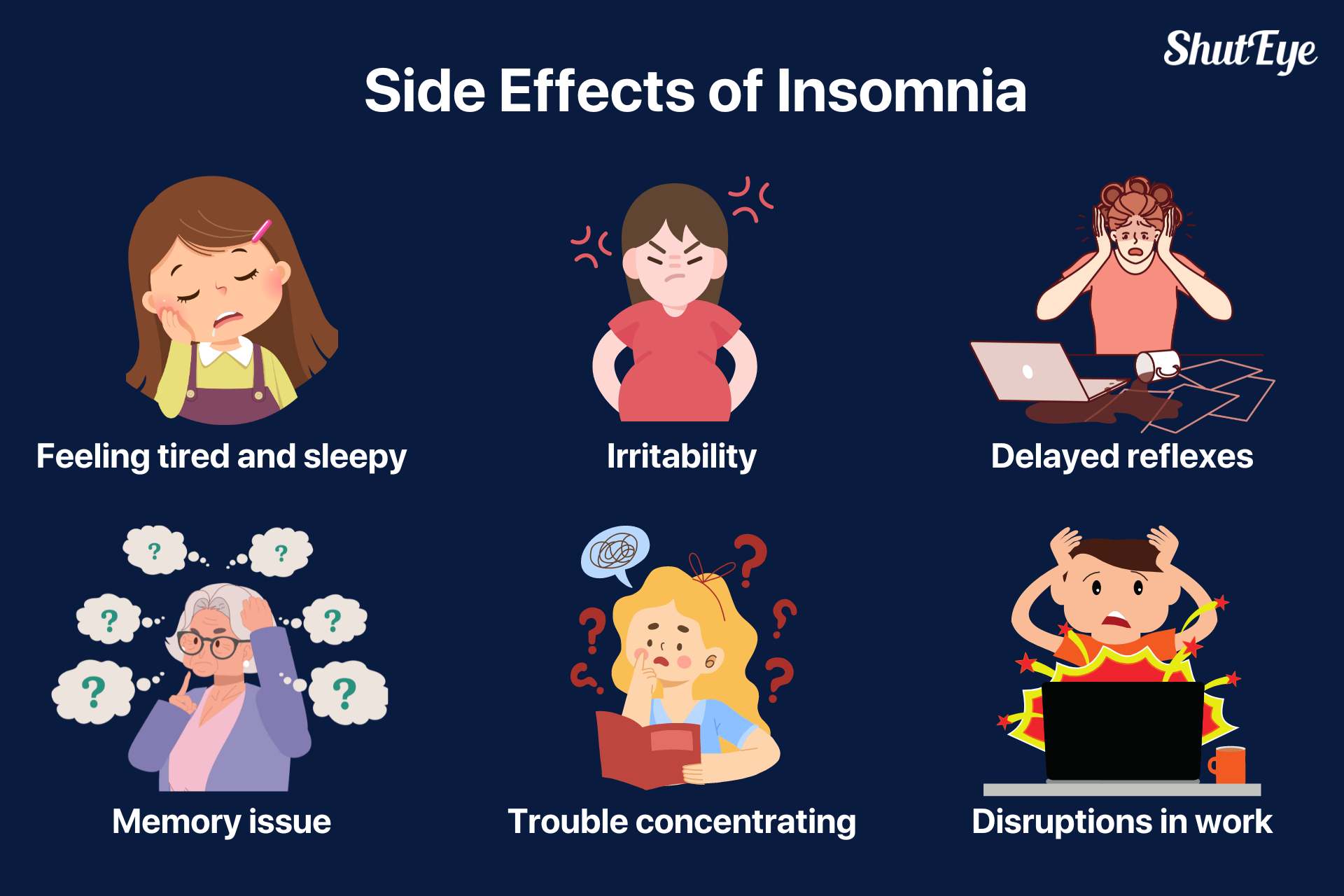
Insomnia is a sleep disorder characterized by persistent trouble falling asleep, staying asleep, reduced sleep duration, disrupted sleep or waking up early, decreased sleep quality, and impaired daytime functioning despite adequate rest and an appropriate sleep environment. Typical symptoms of poor daytime functioning include fatigue, depression or irritability, difficulty concentrating, memory loss, limited social or occupational skills, and reduced learning ability.

Insomnia manifests in two main forms:
Based on duration, experts classify insomnia as follows:
Insomnia can be caused by various triggers and risk factors. The Spielman’s 3P Model of insomnia is a popular theory that describes how insomnia occurs and how acute insomnia becomes chronic insomnia. Among these, the individual susceptibility plays an important role.
They include genetic susceptibility to insomnia or related factors associated with enhanced basal metabolic rate of an individual, hyper-responsiveness and sleep wakefulness-related alterations in the neurotransmitter system.
Moreover, psychological factors include a personality tendency to excessive worry or overthink about some issues. People with a high susceptibility to insomnia have a lower physiological threshold for stimulus events leading to insomnia. For instance, the stimulus may not cause insomnia in others but may trigger it in individuals with a high susceptibility to insomnia.
These events or “triggers” usually relate to stressful life events, including work stress, death of a beloved, pregnancy, divorce, job loss or other significant life events. These stressful events can lead to short-term or persistent sleep disorders.
Staying up late and engaging activities like exercising or consuming coffee and alcohol close to bedtime can contribute to insomnia in adults. Additionally, irregular sleep schedules, prolonged time spent in bed, and inappropriate napping can further disrupt nighttime sleep. In children, resistance to sleep may manifest through behaviors such as climbing out of bed, speaking, crying, and seeking attention, often requiring specific actions like rocking, feeding, or parental presence in the bedroom to facilitate returning to sleep after waking up at night.
Environments with excessive noise, high or low temperature, low pressure, and lack of oxygen (i.e., plateau) can cause insomnia.
Mental health conditions, especially mood disorders and anxiety disorders, can increase the risk of chronic insomnia. Likewise, many physical diseases, accompanied by pain (rheumatic diseases), dyspnea or orthopnea (cardiovascular or pulmonary diseases), nocturia (congestive heart failure use of diuretics, benign prostatic hyperplasia, untreated obstructive sleep apnea), and the adverse effects of drugs used in the chronic disease treatment, may cause sleep problems.
Insomnia may relate to the application or withdrawal of certain drugs or substances. Common drugs and substances that may cause insomnia include anticonvulsants, antianxiety and antidepressant medication, β-blockers, alcohol, narcotics, and marijuana.
These are behaviors performed by individuals to reverse or deal with sleep disorders like insomnia, but they might aggravate it instead of improving sleep.
These factors include the following three aspects of behaviors and sleep habits:
These irrational thoughts may lead to excessive worrying about the adverse effects of insomnia, increase pressure, trigger anxiety, disrupt the normal sleep process, and make insomnia and dreaminess worse, resulting in a vicious circle.

Insomnia can affect daytime functions and lead to fatigue and cognitive impairment. Insomnia can also lead to other physical diseases, such as cardiovascular diseases, metabolic and endocrine abnormalities, etc. Furthermore, long-term Insomnia may also impact survival time. Therefore, individuals with these issues should immediately seek medical help.
Individuals should cautiously recall the beginning and development of insomnia, including the triggers, treatment and response and the medications they have been taking in the past month. They should provide information about the condition relating to physical discomfort or disease, previous consultation experience, test results and treatment, and any history of drug allergy.
Sleep specialists should obtain a comprehensive medical history of sleep habits and practices for dealing with insomnia and other abnormal sleep behaviors. Similarly, they should investigate the dream enactment behaviors, any uncomfortable sensations, and spontaneous movements of the limbs before and during sleep.
The following clinical symptoms can diagnose insomnia:
Once insomnia diagnosed, individuals should use professional Cognitive-Behavioral Therapy (CBT) and psychological counseling or medication to help improve sleep quality. They should not excessively worry about sleep, focus on whether daytime functioning is impaired. Excessive worrying may worsen insomnia increasing psychological stress and making it harder to recover from the disorder. Many studies demonstrate that after systematic CBT, the insomnia symptoms of nearly half of individuals can improve substantially.
A combined non-pharmacological treatment of cognitive psychotherapy, stimulus control, and sleep restriction—combined or not with relaxation therapy—is equally essential as the pharmacological treatment of insomnia.
Psychotherapy generally includes psychological counseling, explanation, and guidance, where patients can learn basic knowledge about sleep and reduce needless anticipatory anxiety. They should correct misperceptions change poor sleep habits, and wrong behaviors in dealing with insomnia.
It’s worth noting that there are various commercially available CBT insomnia apps on the market. We have meticulously curated a list of the best ones, tested through scientifically valid methods to ensure their efficacy.
Due to individual differences, there is no absolute best, fastest, and most effective medication. In addition to commonly used over-the-counter medications other medications should be prescribed under medical supervision.
First, individuals should take sleeping pills under the guidance of a professional sleep physician. Second, it is vital to understand the timing of sleeping pills taking effect and acting after oral administration. For example, they can take fast-acting drugs such as zolpidem and zaleplon after lying on the bed and slow-acting drugs 30-60min before bedtime. Likewise, they may take melatonin 1.5-2 hours before bedtime too. The action duration of drugs is generally shorter than the expected sleep time, but some individuals may take them late at night or early in the morning. As a result, the drug is still effective when waking up, which may impair daytime functioning.
Family or caregivers should administer older people taking sleep pills—especially those with muscle relaxation effects—to prevent falls at night or during the day.
See also:
Can you die from lack of sleep?
It is essential to improve the surrounding environment and poor sleep hygiene habits, maintain a balanced diet to treat insomnia. Moreover, it is vital to exercise moderately to relax the body and relieve stress, downplay or ignore unhappy factors, and reduce excessive anxiety about private or public events.
Maintaining a room temperature of about 20℃ may help individuals sleep better. In addition, a quiet environment can be conducive to improving sleep quality. Adjust the bed, bedding, and pillow to make it comfortable and satisfying and create an excellent sleeping ecosystem. Taking a bath before going to bed is vital. A hot bath before bedtime can help the body and mind to relax. Lying in bed after a hot bath when body temperature returns to normal can help to fall asleep.
Under the guidance of a physician, individuals should keep their sleep diary to record their bedtime, wake-up time, practical sleep time factors affecting sleep, medication, and subjective feelings and scores of sleep. It allows the physician to estimate an individual’s sleep latency time, sleep maintenance, and sleep routine.
We recommend integrating a dedicated sleep-tracking app to enhance this monitoring process. ShutEye® App is a prime example of such a tool. It proves to be an ideal solution not only for tracking sleep but also for detecting patterns associated with insomnia, offering a more comprehensive approach to sleep management.
From the perspective of preventing the disease, individuals should try the following home remedies and lifestyle changes to avoid insomnia:
Insomnia is a pervasive sleep disorder affecting millions worldwide. However, by understanding its causes and symptoms, we can arm ourselves with the tools to reclaim our restful sleep. From Cognitive Behavioral Therapy to lifestyle changes, a variety of strategies exist to combat Insomnia.
Remember, the journey to improved sleep begins with awareness and proactive steps towards change!
NHLBI. 13 December 2011. Archived from the original on 11 August 2016. Retrieved 9 August 2016, from https://web.archive.org/web/20160811091424/http://www.nhlbi.nih.gov/health/health-topics/topics/inso/diagnosis
"What Causes Insomnia?". Retrieved 24 April 2019, from https://www.sleepfoundation.org/insomnia/what-causes-insomnia
"What Is Insomnia?". Health Topics. NHLBI. 24 March 2022. Archived from the original on 28 July 2016. Retrieved 26 November 2023, from https://www.nhlbi.nih.gov/health/insomnia "Types of Insomnia".
Sleep Foundation. 2020-08-31. Retrieved 2022-07-15, from https://www.sleepfoundation.org/insomnia/types-of-insomnia