

Many various factors can contribute to someone not being able to sleep well at night. Besides making changes to your lifestyle and sleeping habits, some may turn to sleeping pills and medication as a temporary solution. But, the question is— how do you know which is the right sleep medication for you to take?
In this article, we’ll explore the different types of sleep medications available, the benefits and risks along with some alternative solutions if you’re looking to avoid the use of sleep aids.

Sleep medication, in broad terms, is a type of medication that helps individuals to fall asleep and stay asleep at night. It is often recognized to be synonymous with sleeping pills.
Sleeping pills are medications used to help people with sleep disorders such as insomnia or those with trouble sleeping to be able to sleep soundly at night.
They can be classified into two main categories— prescription sleeping pills and non-prescription sleeping pills. From here, it is further broken down into different sub-categories based on their chemical structure and mechanism of action [1].
Under prescription sleeping pills, there are many different types of medications that can be classified as sedative-hypnotics. These are medicines that work by increasing the activity of GABA, a neurotransmitter that sends signals to the brain [2].
Benzodiazepines are the most common type of sedative-hypnotics that produce sedation, muscle relaxation and reduce anxiety which helps you fall asleep faster. They are generally recommended as a short-term treatment option for insomnia. Some approved benzodiazepines include estazolam, flurazepam, temazepam, triazolam [3], [4].
Other common prescription sleeping pills include zopiclone and zolpidem, where the effect may be similar to benzodiazepines.

There are also non-prescription sleeping pills or over-the-counter (OTC) sleep aids that are widely available to those looking for short-term relief but without having to deal with serious side effects. Standard non-prescription medicines rely on antihistamines as a primary ingredient to promote drowsiness.
Common sleeping aids that you’ll find over the counter include [3]:
The main benefits of taking these sleep medicines are that they can either help you fall asleep stay asleep, or both. However, it’s also important to note that most of them can lead to dependency when used in the long run.
In addition, depending on the type of medication that you are using, there may be some side effects including [5]:
When considering taking sleep aids, it’s important to prioritize your safety to avoid any risks or complications. Some key factors you want to keep in mind would be:
Older adults and pregnant individuals should be especially cautious when it comes to taking any sleep supplements as there are increased risk and higher sensitivities.


For those who don’t wish to use sleeping pills or any form of medication due to the potential side effects, you may consider the use of solutions such as cognitive behavioral therapy for insomnia (CBT-I) or cultivating good sleep habits.
Cognitive behavioral therapy for insomnia (CBT-I) is a treatment method that targets sleep difficulties and behaviors that contribute to this sleep disorder over a few sessions [6]. It is also commonly used as a first-line treatment for chronic insomnia in adults [7].
Alternatively, you can also practice good sleep habits such as following a consistent sleep schedule, limiting daytime naps, managing stress or creating a relaxing bedtime routine, to name a few. Good sleep habits can contribute to lowered stress levels and result in improved sleep quality.
In short, sleeping pills can be useful in managing insomnia symptoms such as trouble falling asleep. However, it is important to note that they are only temporary solutions. Identifying the underlying cause and creating good sleep habits can help to promote better sleep in the long term.
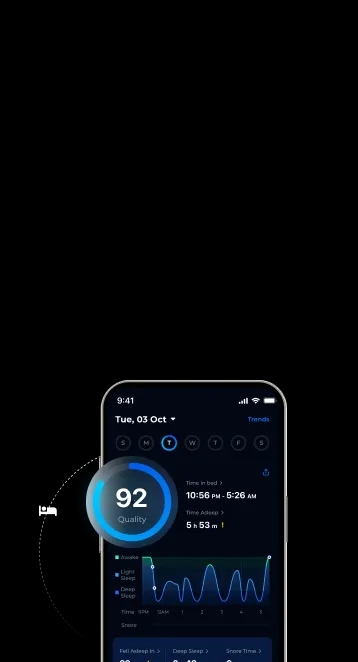
Explore and learn sleep methods and tools to improve your sleep experience with the ShutEye® app. ShutEye® is a patented sleep-tracking app that tracks your sleep and creates a personalized sleep plan for you to achieve healthy rest. Try it FREE!
Akkayagorn, L. (2023) Sleeping pills - Side effect & Treatments [online]. Available at: https://www.medparkhospital.com/en-US/lifestyles/sleeping-pills
American Academy of Sleep Medicine (2024) Digital cognitive behavioral therapy for insomnia: Platforms and characteristics [online]. Available at: https://aasm.org/digital-cognitive-behavioral-therapy-for-insomnia-platforms-and-characteristics/
Better Health Channel (2023) Benzodiazepines [online]. Available at: https://www.betterhealth.vic.gov.au/health/healthyliving/benzodiazepines
Khan, S. (n.d.) How Do Sedative/Hypnotics Work? [online]. Available at: https://www.rxlist.com/sedativehypnotics/drug-class.htm
Mayo Clinic (2022) Prescription sleeping pills: What's right for you? [online]. Available at: https://www.mayoclinic.org/diseases-conditions/insomnia/in-depth/sleeping-pills/art-20043959
Smith, M. and Robinson, L. (2025) Sleeping Pills and Natural Sleep Aids [online]. Available at: https://www.helpguide.org/wellness/sleep/sleeping-pills-and-natural-sleep-aids
Walker, J., Muench, A., Perlis, M. L., & Vargas, I. (2022) Cognitive Behavioral Therapy for Insomnia (CBT-I): A Primer. Klinicheskaia i Spetsial'naia Psikhologiia = Clinical Psychology and Special Education, 11(2), 123. Available at: https://doi.org/10.17759/cpse.2022110208