

Have you ever had a loved one telling you that you were behaving weirdly in your sleep last night? You could have been flailing your hands around or saying something all of a sudden while dreaming. This may be an indicator that you have REM sleep behavior disorder.
While REM sleep behavior disorder is not all that common, it can cause injury to yourself or a bed partner if it happens to be a violent dream.
During sleep, your brain moves through several different stages. REM (Rapid Eye Movement) sleep is one of the stages of sleep cycle, in which your eyes move around rapidly in a range of directions and most of your dreams occur in this period.
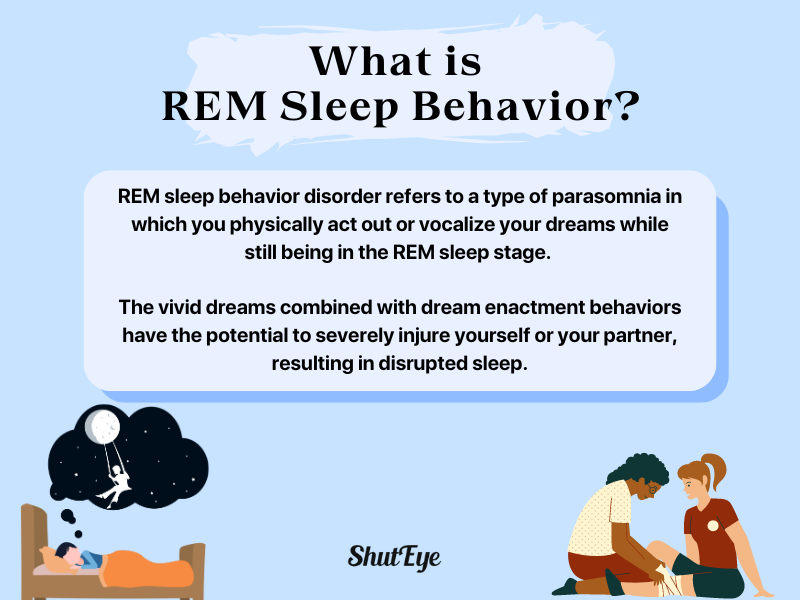
REM sleep behavior disorder refers to a sleep disorder in which you physically act out or vocalize your dreams while still being in the REM sleep stage. It is a type of parasomnia.
The vivid dreams combined with dream enactment behaviors have the potential to severely injure yourself or your partner, resulting in disrupted sleep.
The prevalence of spontaneous REM sleep behavior disorder (RBD) is said to be about 1% of the general population and 2% in older adults [1].
This sleep disorder is typically an indicator of more serious conditions such as Parkinson disease, multiple system atrophy and lewy body dementia, affecting as high as 76-81% of individuals.
Some of the common symptoms of REM sleep behavior disorder (RBD) include:
The exact cause of RBD is unknown. Animal studies suggest that it has to do with certain neural pathways in the brain. During normal REM, nerve pathways in the brain that prevent muscles from moving are active, which could keep your body temporarily “paralysis”. However, with RBD, these pathways might no longer work and you may physically act out your dreams.
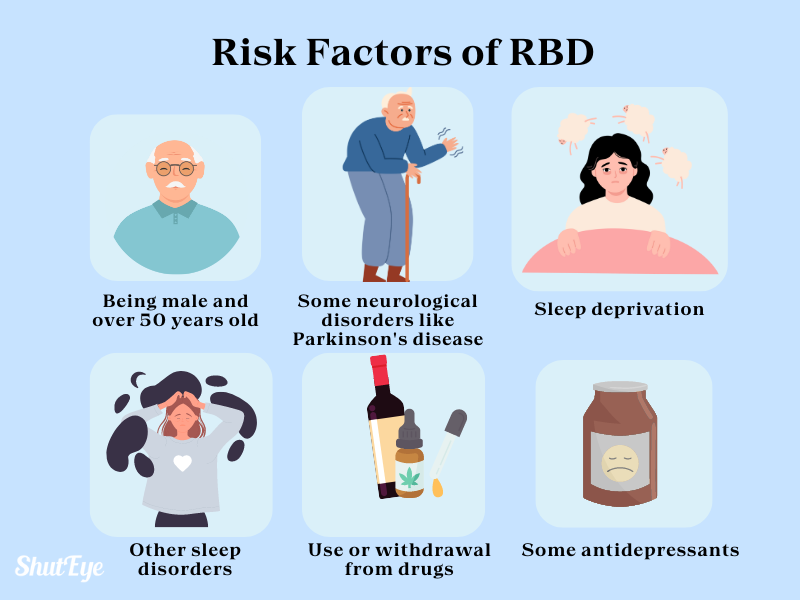
Risk factors of RBD may include:
There are many conditions that may seem similar to REM sleep behavior disorder as they mimic the same symptoms. For example, the movements that happen while in REM sleep could be aligned with obstructive sleep apnea (OSA).
Limb twitching could resemble periodic leg movements (PLMS). Not only that, but dream enactment behavior is also not an exclusive symptom to patients with RBD. Other conditions that are associated with dream enactment behavior are:
As dream enactment behavior is not exclusive to this condition, RBD cannot be determined solely based on medical history or recorded events.
According to the third edition of the International Classification of Sleep Disorders (ICSD-3), to properly diagnose someone with RBD, you need to fulfill these criteria [1]:
A team approach involving clinical sleep medicine specialists, neurologists, and other healthcare providers ensures accurate diagnosis and appropriate management. Early detection and intervention are crucial for improving outcomes and reducing complications.
REM Sleep Behavior Disorder (RBD) can lead to various complications, both for the individual experiencing the disorder and potentially for their sleep partners or others nearby. Some of the complications include:
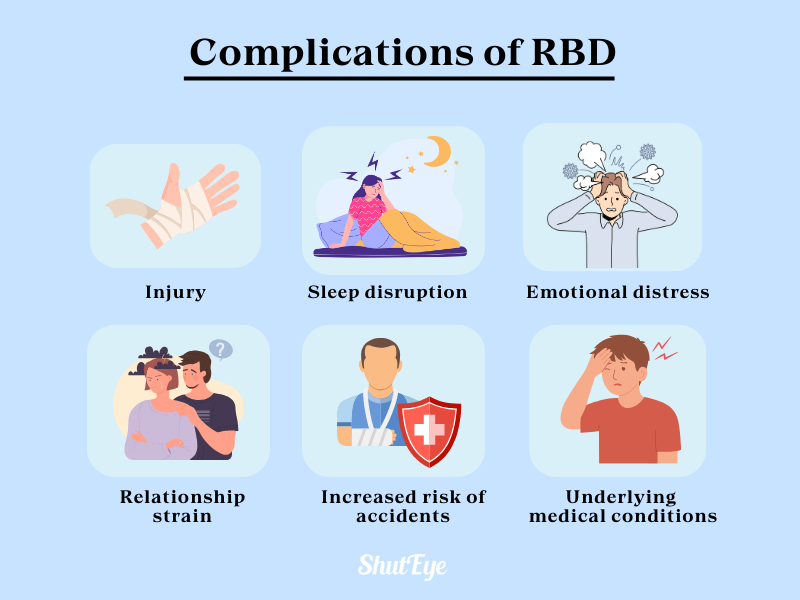
These complications highlight the importance of seeking medical evaluation and treatment for individuals experiencing symptoms of the disorder. Management strategies may include lifestyle modifications, medication, or other interventions aimed at reducing the frequency and severity of RBD episodes and improving overall sleep quality and safety.
Related content:
Managing this condition may involve a combination of lifestyle changes and medication such as:

A good lifestyle is conducive to improving the quality of sleep and decreasing the risk of suffering RBD. As much as possible, try to maintain a consistent sleep schedule. Sleep deprivation can increase the occurrence of RBD.
You can also monitor the quality of your sleep with sleep-tracking apps such as ShutEye. Tracking your sleep is the first step to knowing how you can improve your sleep.
A number of medications have proven effective in cases of RBD depending on which symptoms present. Currently, two main drugs are used to effectively treat RBD including melatonin and clonazepam.
However, you want to make sure that you are diagnosed with REM sleep behavior disorder by a sleep specialist before taking medications such as clonazepam. If it turns out to be obstructive sleep apnea (OSA) instead of RBD, taking clonazepam could worsen the condition.
During an episode, you would be completely unaware of your surroundings. If it turns out to be a violent dream, you may wound up accidentally hurting yourself or your bed partner.
This is why it is recommended that you ensure that your bedroom environment is physically safe by:
Therefore, while REM Sleep Behavior Disorder can be potentially dangerous, it can be managed with early diagnosis and the right treatment. It is important to consult a professional sleep doctor when you suspect that you are exhibiting abnormal behaviors while asleep.
By doing so, slowly but surely, you are on your way to better quality sleep.
REM Sleep: Why It Matters For Health
The Importance of REM Sleep and Dreams in the Sleep Cycle
Khawaja I, Spurling BC, Singh S. REM Sleep Behavior Disorder. [Updated 2023 Apr 24]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK534239/