
If you’re struggling with unexplained daytime sleepiness or sudden muscle weakness, understanding narcolepsy is key. This comprehensive guide dives into the diagnosis, treatment, symptoms, and causes of narcolepsy.
By empowering yourself with knowledge on managing its impact, you can navigate daily challenges. From specialist evaluations to coping strategies, stay informed and proactive in your healthcare journey.
Narcolepsy is a chronic neurological disorder characterized by excessive daytime sleepiness and uncontrollable episodes of falling asleep during the day. People who have narcolepsy often experience sudden and unexpected sleep attacks, which can occur during various activities such as working, studying, or even driving.
In addition to excessive daytime sleepiness, narcolepsy also involves similar symptoms such as cataplexy (sudden loss of muscle tone), sleep paralysis (temporary inability to move or speak upon waking or falling asleep), hypnagogic hallucinations (vivid dream-like experiences), and disrupted sleep at night. This condition can significantly impact daily functioning and quality of life, but with proper diagnosis and management, adults with narcolepsy can lead fulfilling lives.
Understanding the etiology of narcolepsy is essential for identifying potential risk factors. Narcolepsy is believed to be linked to changes in the brain affecting sleep regulation. Nearly all cases with cataplexy exhibit low hypocretin-1 levels, suggesting a role for this neurotransmitter in the disorder.
Genetic and environmental factors may contribute to the development of narcolepsy, impacting both children and adults equally. When diagnosed with narcolepsy, treatment for narcolepsy focuses on symptom management, with medications like modafinil, armodafinil, and sodium oxybate playing a crucial role. Lifestyle adjustments, such as incorporating naps and maintaining healthy sleep habits, are also recommended.
Proper diagnosis aids in differentiating between narcolepsy types and tailoring effective treatment plans to improve quality of life.

Understanding the classification and manifestations of narcolepsy is crucial for identifying the condition’s specific characteristics and symptoms accurately. Narcolepsy is a sleep disorder where individuals can unexpectedly fall asleep at any time, impacting their daily lives. It’s classified into two types:
Symptoms may include excessive daytime sleepiness, cataplexy (sudden muscle weakness), hallucinations, and sleep paralysis. Medical professionals can conduct various tests on people with narcolepsy to diagnose narcolepsy accurately, and treatments like medication and lifestyle adjustments can help alleviate symptoms and improve the quality of life for individuals with narcolepsy.
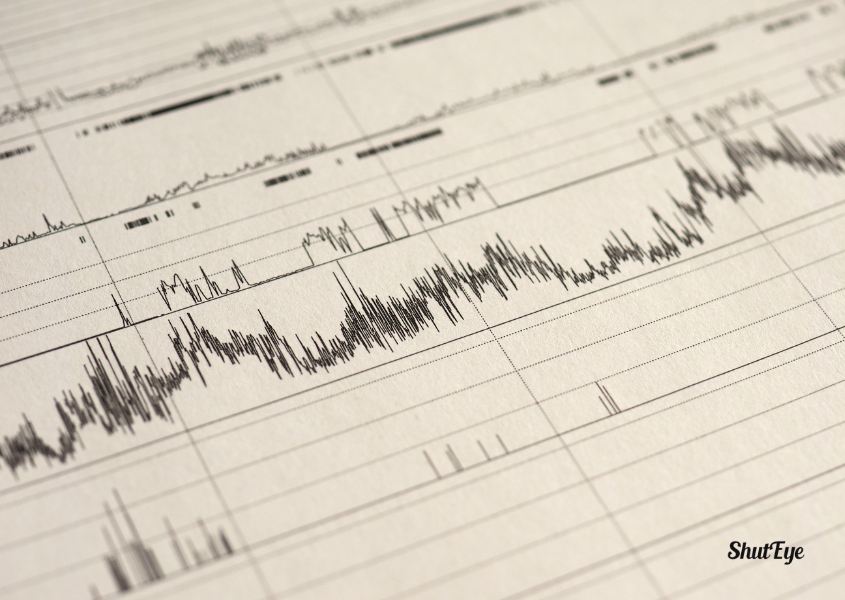
To properly diagnose narcolepsy and differentiate between its types, medical professionals rely on specific criteria and tests. Diagnosis of narcolepsy often involves a thorough physical examination, evaluation of medical history, and specialized sleep monitoring tests such as polysomnogram (PSG) and multiple sleep latency test (MSLT).
These tests help in identifying characteristics like rapid eye movement (REM) sleep abnormalities and excessive daytime sleepiness (EDS) that are indicative of narcolepsy. Additionally, lumbar puncture to measure hypocretin levels can aid in confirming the diagnosis and distinguishing narcolepsy from other conditions causing daytime drowsiness.
Proper diagnosis is crucial for initiating appropriate treatment strategies tailored to manage symptoms effectively and improve the quality of life for individuals living with narcolepsy.
Diagnosis of narcolepsy is crucial as it paves the way for tailored treatment plans that effectively manage symptoms and enhance quality of life. While narcolepsy is not officially listed as a disability by the Social Security Administration (SSA), patients with narcolepsy can still seek disability benefits based on the severity of their symptoms. Once diagnosed, various treatment options can help you manage narcolepsy. Medications such as modafinil and sodium oxybate can alleviate daytime sleepiness and cataplexy.
Additionally, lifestyle adjustments like maintaining a regular sleep schedule, incorporating short naps during the day, and avoiding stimulants before bedtime can aid in symptom management. Safety precautions, especially while driving, are vital to ensure your well-being.
As you navigate the impact of narcolepsy on your daily life, it’s crucial to recognize the importance of tailored treatment plans and lifestyle adjustments for better symptom management. The effects of narcolepsy can be profound, influencing various aspects of your daily routine and overall well-being.
Here are some key points to consider:
When managing narcolepsy, incorporating effective coping strategies is essential for improving daily functioning and quality of life.
To navigate the challenges of narcolepsy management, consider the following:
Practical Coping Strategies:
Emotional Coping Techniques:
These coping strategies can complement medical treatments and help you better manage narcolepsy symptoms in your daily life.
Explore current studies on narcolepsy and its underlying mechanisms to uncover new treatment possibilities. Recent research on narcolepsy has delved into understanding the intricate factors contributing to this disorder. By investigating the genetic, environmental, and immunological aspects of narcolepsy, researchers aim to develop more effective treatments tailored to individual needs. Below is a table summarizing key insights from recent studies:
| Research Insights | Focus Areas | Potential Impact |
|---|---|---|
| Genetic Studies | Identifying genetic markers linked to narcolepsy | Personalized treatment approaches |
| Immunological Research | Examining immune system involvement in the disease | Novel immunotherapies for management |
| Sleep Biology Exploration | Investigating abnormalities in sleep regulation | Enhanced understanding of narcolepsy |
These ongoing studies offer hope for advancements in narcolepsy management and treatment options.
Continuing to delve into the topic of narcolepsy, you can access valuable narcolepsy awareness and support resources for comprehensive information and assistance.
Narcolepsy Network and National Sleep Foundation offer educational materials and community support for individuals and families affected by narcolepsy.
Platforms like Inspire and Reddit communities provide spaces for sharing experiences, asking questions, and receiving peer support regarding narcolepsy symptoms, diagnosis, and treatment options.
These resources can be instrumental in navigating the challenges associated with narcolepsy, offering a sense of community, understanding, and guidance throughout your journey with this neurological disorder.
For patients living with narcolepsy, understanding the long-term outlook and prognosis is crucial for managing this chronic neurological condition. When diagnosed, the cause of narcolepsy is often linked to genetic and environmental factors affecting hypocretin production in the brain.
While there is currently no cure for narcolepsy, treatments aim to manage symptoms and improve quality of life. It’s essential to differentiate between the types of narcolepsy, such as Type 1 with cataplexy or Type 2 without, to tailor treatment effectively. Long-term management strategies, including medications and lifestyle adjustments, can help individuals cope with narcolepsy and lead fulfilling lives despite the challenges it presents.
Moreover, recent studies have explored the intriguing connection between ADHD and narcolepsy, shedding light on potential overlaps in symptoms and underlying mechanisms.
| Aspect | Description | Emotional Impact |
|---|---|---|
| Narcolepsy Diagnosed | Genetic & environmental factors contribute to diagnosis. | Understanding the root cause can be reassuring. |
| Cause of Narcolepsy | Hypocretin production affected by genetic and environmental factors. | Knowing the cause can provide clarity and direction. |
| Type of Narcolepsy | Type 1 with cataplexy or Type 2 without cataplexy. | Understanding the type can guide treatment decisions. |
| Treat Narcolepsy | Management through medications and lifestyle adjustments. | Hope for symptom control and improved quality of life. |
| Cure for Narcolepsy | No current cure; focus on symptom management. | Realistic expectations and the importance of ongoing care. |
In conclusion, navigating the complexities of narcolepsy requires knowledge, proactive management, and support.
By understanding the symptoms, seeking a proper diagnosis, exploring treatment options, and utilizing coping strategies, you can better manage the impact of narcolepsy on your daily life.
Stay informed, stay engaged, and remember that you aren’t alone in facing this neurological disorder.
With the right resources and support, you can effectively navigate the challenges posed by narcolepsy and maintain a positive outlook for the future.
National Institute of Neurological Disorders and Stroke (NINDS). (n.d.). Narcolepsy. Retrieved from https://www.ninds.nih.gov/health-information/disorders/narcolepsy
Wilenius L, Partinen M. Attention-Deficit/Hyperactivity Disorder Patients May Have Undiagnosed Narcolepsy. Cureus. 2020 Jun 4;12(6):e8436. doi: 10.7759/cureus.8436. PMID: 32642351; PMCID: PMC7336577.
Pizza, F., Franceschini, C., Peltola, H., Vandi, S., Finotti, E., Ingravallo, F., Nobili, L., Bruni, O., Lin, L., Edwards, M. J., Partinen, M., Dauvilliers, Y., Mignot, E., Bhatia, K. P., & Plazzi, G. (2013). Clinical and polysomnographic course of childhood narcolepsy with cataplexy. Brain: A Journal of Neurology, 136(Pt 12), 3787–3795. https://pubmed.ncbi.nlm.nih.gov/24142146/
Thorpy, M. J., & Krieger, A. C. (2014). Delayed diagnosis of narcolepsy: Characterization and impact. Sleep Medicine, 15(5), 502–507. https://pubmed.ncbi.nlm.nih.gov/24780133/
Ollila, H. M. (2020). Narcolepsy type 1: What have we learned from genetics? Sleep, 43(11), zsaa099. https://pubmed.ncbi.nlm.nih.gov/32442260/