

Ever woken up from a terrifying dream that felt realistic? Have you ever experienced talking in your sleep or sleepwalking? If you’ve ever experienced any of these, chances are you’ve just had parasomnia.
Parasomnia is a mysterious sleep disorder that can be quite unpredictable, affecting not just you but also your loved ones. What causes these strange events and how can they be managed? Keep reading to find out!
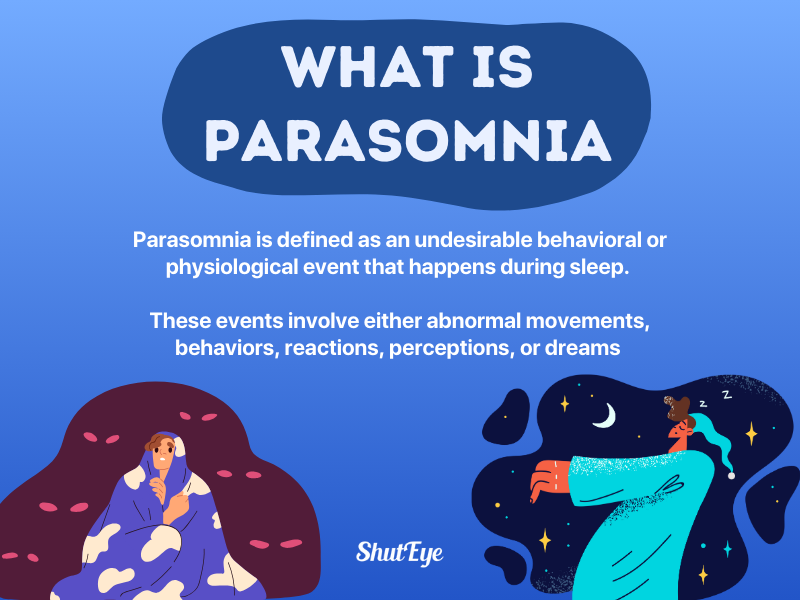
Parasomnia is defined as an undesirable behavioral or physiological event that happens during sleep. These events involve either abnormal movements, behaviors, reactions, perceptions, or dreams [1].
Parasomnias typically occur during REM (rapid eye movement) sleep and non-REM (non-rapid eye movement) sleep. However, it can also occur while falling asleep, between sleep stages or transitioning from sleep to wakefulness [2].
At the present moment, it is still not clear what causes parasomnia. However, some cases of parasomnia can be attributed to factors like sleep deprivation, genetics, neurological disorders, psychological disorders, post-traumatic stress disorder (PTSD), or side effects from a prescribed medication [3], [4].
There are four stages of sleep that our body would cycle through, throughout the night. These stages are separated into two main categories which are: non-REM (non-rapid eye movement) sleep and REM (rapid eye movement) sleep.
Stage 1 to 3 fall into the Non-REM sleep category while Stage 4 falls into the REM sleep category. There are two main types of parasomnia that fall under these categories, known as REM-related parasomnias and non-REM-related parasomnias [5].
Non-REM-related parasomnias usually involve doing a physical or verbal activity unconsciously. You are likely to not remember it the next day.
REM-related parasomnias occur during REM sleep when your eyes move rapidly under the eyelids and you have an increased heart rate, breathing, and blood pressure.
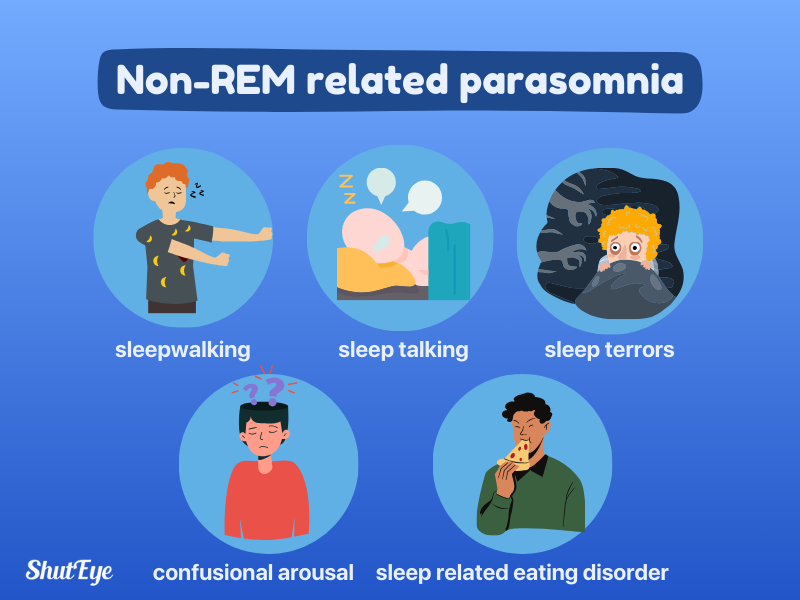
Here are the common traits associated with non-REM-related parasomnias:
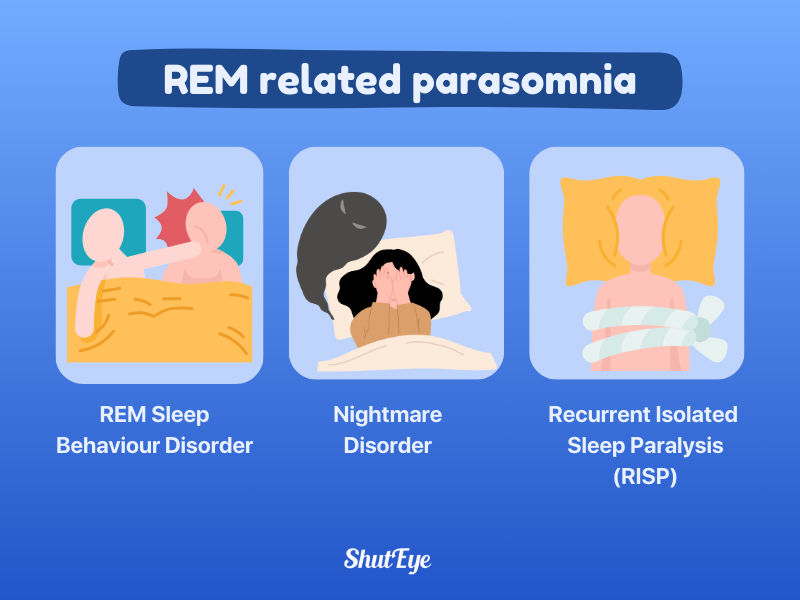
Similarly, for REM-related parasomnias, the common traits are:
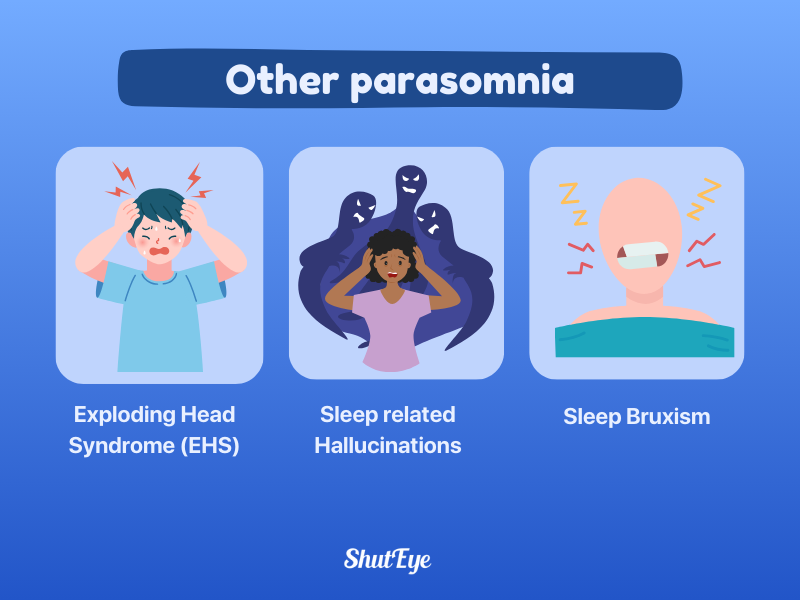
Aside from non-REM-related parasomnias and REM-related parasomnias, other parasomnias occur regardless of the stage of sleep that it is in. It can basically happen anytime during the sleep cycle.
Exploding Head Syndrome (EHS) is a non-harmful parasomnia in which a person experiences hearing a sudden loud noise while asleep, causing abrupt awakenings. Flashes of light and feelings of distress would usually accompany these events.
The sounds are commonly described to be the sounds of explosions, gunshots, or thunder but it can also be any other kind of loud noise. These events do not cause harm or pain.
There are no tests available to properly diagnose exploding head syndrome as well as to determine the cause of it. However, potential triggers are thought to be stress, uncontrolled anxiety, and insomnia [12].
Sleep-related hallucinations or hypnagogic hallucinations are a type of sleep disorder where a person experiences vivid and realistic imagined events upon sleep onset. They are visual hallucinations that may sometimes involve your senses of sound, touch, taste, and smell [13].
It is easily confused with being in a dream as you would be unsure of whether you are awake or asleep. Hallucinations could also be a sign of narcolepsy if it occurs during the day.
Sleep bruxism, also known as teeth grinding, is the involuntary clenching of your jaw and grinding of your teeth while asleep.
It affects an estimated 15 to 40% of children and 8-10% of adults. The causes of sleep bruxism could be due to stress, anxiety, lifestyle factors, and medical or psychological conditions. Teeth grinding also commonly co-occur with obstructive sleep apnea (OSA) and snoring [14].
Parasomnias can be diagnosed by carefully obtaining a thorough clinical history and assessing for characteristics such as time, expression, and present behavior in the individual’s home environment.
Some of the clinical questions asked include questions to rule out sleep deprivation, intoxication or withdrawal, sleep disorders or medical disorders that cause sleep instability, timing of events, and symptoms.
Additionally, a sleep diary or a partner’s account of the events may also help form a diagnosis. If it is a REM-related parasomnia that might cause harm or danger to others, seeing a sleep specialist or doing polysomnography may be necessary.
In most cases, parasomnias would typically resolve on their own by making lifestyle changes such as improving sleep hygiene or sleep habits. Good sleep hygiene and habits include having a consistent sleep schedule, managing stress and anxiety, and getting enough sleep.
However, in some cases, a sleep medicine specialist may recommend a specific treatment based on the diagnosis and severity of the parasomnia.
Here are the common treatment options [15]:

Cognitive Behavioral Therapy (CBT) is a form of psychological treatment that is often used to address sleep disorders, such as parasomnia. It is carried out based on the principles of changing unhealthy thinking or behavioral patterns [16].
An example of cognitive behavioral therapy is image rehearsal therapy. This technique commonly used for nightmare disorder, involves changing the content of the parasomnia into new sets of images. This helps to reduce fear [17].
The primary objective of CBT is to help individuals realize that they are in control of the situation and problems that they are facing.
CBT can be used for nightmare disorder, sleep paralysis, insomnia, confusional arousal, sleepwalking, or night terrors.

Hypnotherapy is defined as a form of psychological therapy that uses hypnosis as a way to change habits.
Based on a long-term study, it was found that hypnosis was most effective at treating parasomnias like nightmares and sleepwalking [18]. Upon completion of 1 to 2 sessions of hypnotherapy and three stages of follow-up post-hypnotherapy, it was found that roughly 40% of the subjects had reported positive changes.
The subjects had either no recurrent episodes of parasomnia or their symptoms were “much improved.” Thus, showing the efficacy of hypnotherapy for specifically nightmare disorder and sleepwalking [19].

Scheduled awakenings are commonly used as a treatment option for young children who deal with frequent parasomnia events [20].
Approximately 40% of children would suffer from sleep problems at some point in their childhood. One of the most common being sleepwalking. As a child transitions from slow-wave sleep to the next sleep cycle, they may become caught between sleep and wakefulness.
This partial arousal state causes sleepwalking to occur. Scheduled awakening is thought to help by waking a child at least 1.5 hours before they would experience the partial arousal parasomnia, as a way of disrupting sleep staging.

The use of medications may be considered when parasomnia occurs frequently, causes extreme anxiety, or has the potential to put someone else at risk.
Common medications prescribed for adults dealing with parasomnia are benzodiazepines, tricyclic antidepressants, or melatonin supplements to reduce episodes.
Melatonin is an alternative first-treatment option for REM-related parasomnia compared to benzodiazepines or antidepressants. It is rarely a recommended treatment option for children. Like all other medications, it’s important to consult with a sleep specialist before using any supplements in case of contraindications or improper use [22].
Therefore, it can be understood that parasomnia is an abnormal behavior or movement that happens during sleep. Severe cases may require polysomnography and prescribed medications. In most cases, it is not harmful and can be easily treated by making changes to your sleep habits or using psychotherapy methods.
Discover ways to improve your sleep hygiene and sleep habits with the ShutEye® app today. ShutEye® is an all-in-one sleep-tracking app that tracks your sleep and offers personalized insights for better sleep.
American Academy of Sleep Medicine (2007) Hypnosis may help people with parasomnias such as nightmares, sleepwalking [online]. Available at: https://sleepeducation.org/hypnosis-help-parasomnias-nightmares-sleepwalking/
American Psychological Association (2015) Scheduled Awakenings for Disorders of Arousal (Parasomnias) [online]. In Pediatric Sleep Problems: A Clinician’s Guide to Behavioral Interventions. Available at: https://www.apa.org/pubs/books/supplemental/pediatric-sleep-problems/Scheduled_Awakenings_for_Disorders_of_Arousal.pdf
American Psychological Association (2017) What is Cognitive Behavioral Therapy? [online]. available at: https://www.apa.org/ptsd-guideline/patients-and-families/cognitive-behavioral
Fariba KA, Tadi P. Parasomnias. [Updated 2023 Jul 17]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available at: https://www.ncbi.nlm.nih.gov/books/NBK560524/
Faap, D. R. N. M. M. (n.d.). Nightmare Disorder: Practice Essentials, Background, Pathophysiology. Available at: https://emedicine.medscape.com/article/914428-overview?form=fpf
John Hopkins Medicine (n.d.) Nightmares and Night Terrors [online]. Available at: https://www.hopkinsmedicine.org/health/conditions-and-diseases/nightmares-and-night-terrors
Khan I, Slowik JM. Exploding Head Syndrome. [Updated 2022 Dec 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available at: https://www.ncbi.nlm.nih.gov/books/NBK560817/
Mundt, J. M., & Baron, K. G. (2021). Integrative behavioral treatment for NREM parasomnias: a case series. Journal of Clinical Sleep Medicine, 17(6), 1313–1316. Available at: https://doi.org/10.5664/jcsm.9186
Ramos, D. F., Magalhães, J., Santos, P., Vale, J., & Santos, M. I. (2019). RECURRENT SLEEP PARALYSIS - FEAR OF SLEEPING. Revista paulista de pediatria : orgao oficial da Sociedade de Pediatria de Sao Paulo, 38, e2018226. Available at: https://doi.org/10.1590/1984-0462/2020/38/2018226
Reid, S. (2024) Parasomnias Types, Causes, and Symptoms [online]. Available at: https://www.helpguide.org/wellness/sleep/parasomnias-types-causes-and-symptoms
Saito, J. and Skiba, V. (2020) Sleep Eating Disorder [online]. Available at: https://sleepeducation.org/sleep-disorders/sleep-eating-disorder/
Salman EJ, Kabir R. Night Eating Syndrome. [Updated 2022 Sep 14]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available at: https://www.ncbi.nlm.nih.gov/books/NBK585047/
Sen, S. (2023) Parasomnia Facts, Causes, and Types [online]. Available at: https://amerisleep.com/blog/parasomnia/#causes-of-parasomnia
Shaikh, I. and Mathew, R. (2020) Sleep Hallucinations [online]. available at: https://sleepeducation.org/sleep-disorders/sleep-hallucinations/
Stanford Medicine (n.d.) Confusional Arousals [online]. Available at: https://stanfordhealthcare.org/medical-conditions/sleep/nighttime-sleep-behaviors/confusional-arousals.html
Vincent, N., Dirkse, D., Giannouli, E., & McQuarrie, A. (2022). Transdiagnostic cognitive behavioral therapy for nightmares and parasomnias. Journal of Clinical Sleep Medicine, 19(3), 499–509. Available at: https://doi.org/10.5664/jcsm.10374
Winkelman, J. W., & Pavlova, M. (2006). PRIMARY DISORDERS OF SLEEP. Neurology and Clinical Neuroscience, 185-202. Available at: https://doi.org/10.1016/B978-0-323-03354-1.50019-5
Yale Medicine (n.d.) Parasomnias [online]. Available at: https://www.yalemedicine.org/conditions/parasomnias
Yap, A. U., & Chua, A. P. (2016). Sleep bruxism: Current knowledge and contemporary management. Journal of conservative dentistry : JCD, 19(5), 383–389. Available at: https://doi.org/10.4103/0972-0707.190007